Why the US needs fake blood

You've heard of Artificial Intelligence, but how about Artificial Blood? #AB, anyone?
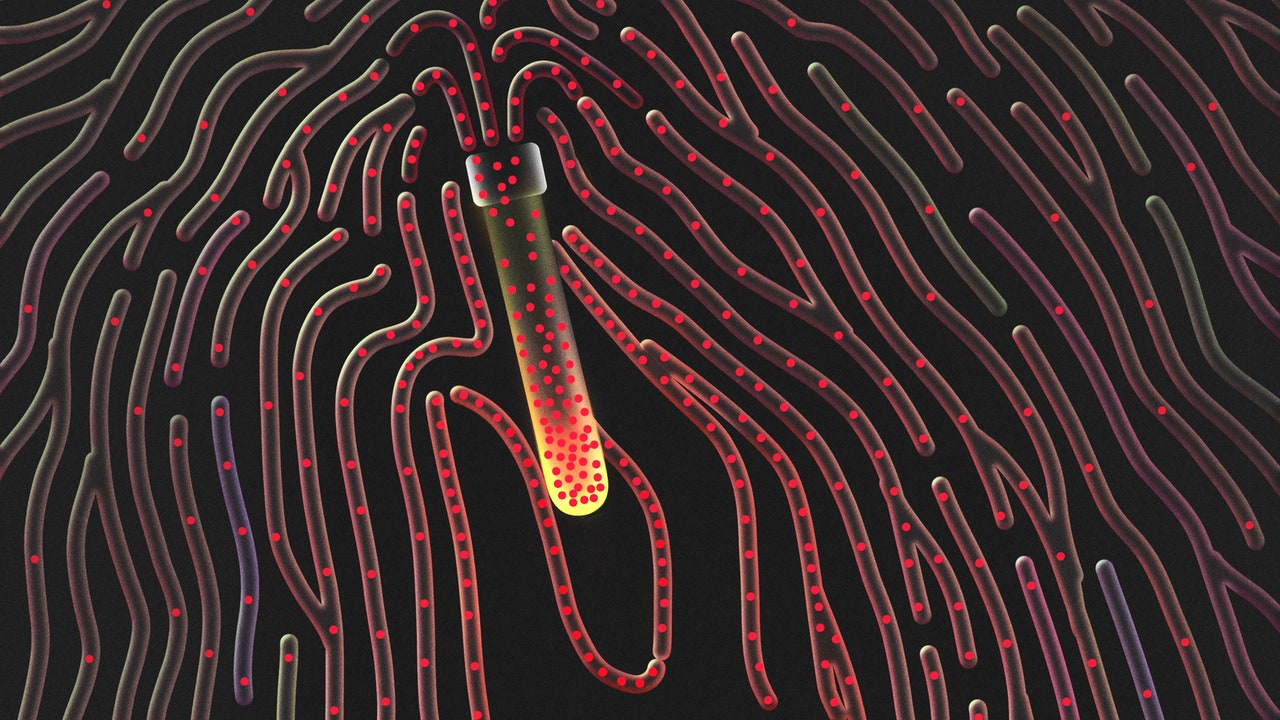
Like the human brain, scientists don't understand everything about human blood or how it works. But we know the building blocks of blood — red and white blood cells, platelets, and plasma — and some of what it does: picks up and drops off oxygen, nutrients, hormones. Blood takes out the toxic garbage while also acting like a thermostat; it's also like a self-cleaning swimming pool washing out with chemicals. Blood protects and warns the body about problems like organ damage (cuts on the skin, say as an example).
Blood brings the harmony — it's a special part of the human body, and hard to imagine creating from scratch outside the millions of years of evolution swirling within us.
But that hasn't stopped some medical labs, bio-lab startups, multiple countries, and the US government from trying to figure blood out and make it. For example, one bio-startup, KaloCyte has invented ErythroMer, a synthetic artificial red blood cell, which they hope will eventually be used as a replacement for the whole blood in the human body. The startup also got funds from a U.S. defense agency in DARPA with $46 million dollars. War, as it so often does, may be a motivator for such a grant and the need for artificial blood. (The Spanish Civil War helped advance storage and transfusion of blood in the 20th century).
https://www.science.org/content/article/ultimate-blood-substitute-us-military-betting-46-million
Blood is needed. A hundred and fifty thousand in the US civilians die each year, more than five million around the world. With an injury, blood loss is the most common reason for preventable death. Blood is needed, too, for clotting platelets in childbirth, surgery, and trauma; many cities often run out during a day, especially given the short shelf life and complicating thawing process needed to use frozen blood.
Out of the 38% of Americans able to donate, only 3% do. You can't sell most of your blood legally in the U.S., and even if you could, the practice would likely exploit the poor.
(Just see what's happened with selling plasma with plasma centers concentrated in poorer zip codes and college towns with hundreds of dollars twice a week).

Simply put, there isn't enough blood. When there is enough, what saves lives is prehospital blood: the blood used out in the field on a highway, home, or riding an ambulance. Blood can be transported in coolers, by drone, stored in ambulances, agencies, blood banks, but the storage and transportation isn't the problem. It's economics.
Nicola Twilley interviewed many for her New Yorker profile on those trying to make artificial blood. John Holcomb, a trauma surgeon told her:
“The problem here is that there’s practically no reimbursement for prehospital blood by insurance and agencies,” Holcomb said. “There’s nothing that has a bigger impact on survival than prehospital blood. Nothing. And yet the major impediment is not logistics—we’ve worked through that. It’s not how to store the blood. It’s reimbursement. And, in our system, if you don’t get reimbursed you don’t do it.”
According to one trial, prehospital blood made a huge difference between life and death. After 30 days, people who received prehospital plasma had a nearly 10% higher chance of living.
https://www.nejm.org/doi/full/10.1056/NEJMoa1802345
So, no matter what you invent, you need to also invent a better system. Before you make a better car, you also need a better road.



Member discussion